The COVID-19 pandemic has changed our day-to-day lives for the past year. The virus is a severe acute respiratory syndrome coronavirus (SARS-CoV-2). Its rapid spread caused over 4 million deaths around the globe, changing the landscape of medicine forever.
Although the clinical features observed in COVID-19 patients mostly affect the respiratory and circulatory systems, there is mounting evidence about the neurological manifestations that impact nearly 30% of COVID-19 patients.
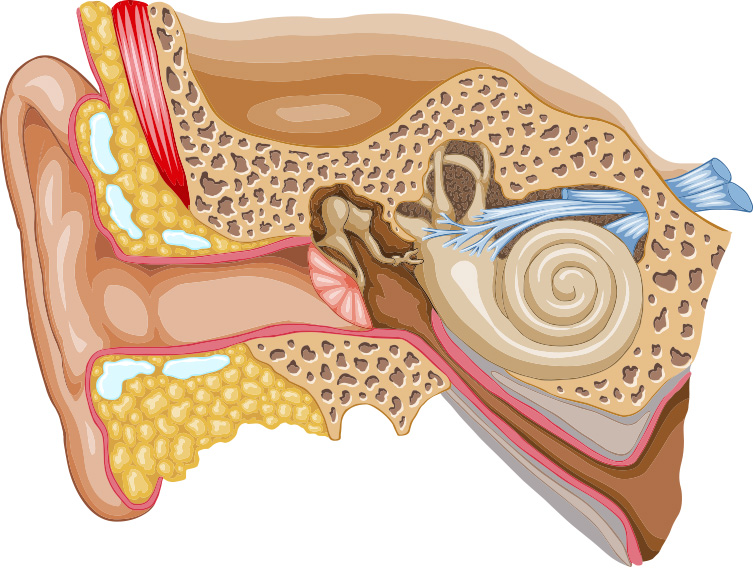
Common symptoms of COVID-19 include cough, fever, fatigue, body aches, and G.I. distress. Neurological symptoms reported in 30% of patients include loss of smell, loss of taste, migraine headaches, and dizziness. This is not surprising since dizziness is associated with viral infections of the inner ear.
Dizziness is a broad term and can mean different things to different patients. Dizziness described as lightheadedness can mean feeling like you are about to faint or feel unsteady when walking. In a study by Viola et al, 18% of COVID-19 patients complained of dizziness. Of those patients, 8% experienced lightheadedness, 8% had imbalance with walking, and 2% felt the true spinning of vertigo. In the study, 23% of patients reported symptoms of tinnitus (ringing in the ear), which was intermittent or constant in nature.
Is dizziness specifically caused by a COVID-19 infection? The quarantine lifestyle that we have been forced to adopt over the last year may also be a factor. The change in normal activity levels has specifically affected our senior population, which was most at risk. They went out much less, limiting their activities to walking around their home—for less than when they were out and about in their communities prior to the pandemic. The reduced socialization activities such as going to the food store, walking around a shop, going to the doctor’s office, and visiting with the family have taken their toll on the senior population, leading to decreased endurance for ambulation and reduced strength. For a population already prone to falls, this consequence of the pandemic can put seniors at higher risk of falling.
In addition, patients who did contract COVID-19 may have impaired breathing, which can cause patients to feel lightheaded with exertion. Inadequate circulation due to COVID-related cardiac problems can cause low blood pressure and impair the amount of oxygen circulated to the brain, which leads to dizziness. These patients would benefit from a supervised exercise program to work on endurance and balance, which can be provided by a Physical Therapist.

Vertigo and Migraine Headaches
Vertigo, a false sense of movement with spinning and feeling off-balance, is something that we commonly treat at WWSPT. We specialize in the care of disorders related to the vestibular system—most commonly vertigo. Since the pandemic began, we have seen an increase in vertigo-associated disorders and migraine-associated vertigo referred to our clinic. Many vertigo-related disorders are in post- COVID patients.
BPPV, a mechanical disorder of the inner ear where crystals are displaced causing acute vertigo, may develop within weeks after a COVID-19 infection, manifesting with short attacks of vertigo and spinning with associated nausea and vomiting. Vestibular Rehabilitation is effective in the treatment of BPPV, with maneuvers designed to move displaced crystals back to the proper place in the inner ear and reduce vertigo attacks.
Headache has been reported as the first symptom in 26% of people with COVID-19, and it presented within 24 hours for 62% of people with the virus. One-quarter of these patients have a headache that resembles a migraine, and 54% experience what resembles a tension-type headache.
Migraine headaches are a common neurological symptom, and changes in lifestyle due to the pandemic can influence the frequency of migraines and headaches. Changes in our work settings and hours, increases in screen time at home, increases in stress, and disruption in sleep, and regular exercise patterns all affect the frequency of migraines. Working at temporary desks and using poor posture can lead to tension headaches and cervical pain. In the early months of the pandemic, we saw many patients in the clinic for whom we were able to help make simple adjustments to their work-from-home setup to reduce migraine headaches.
A vestibular migraine is a common form of migraine that doesn’t always have a headache associated with it but can have other vestibular symptoms such as vertigo, nausea, light and sound sensitivity, and imbalance which are just as disabling as a headache. Many of the same triggers for migraine headaches can cause a vestibular migraine, but it is not as well recognized.
In a small set of post- COVID patients, headaches seem to linger long after the illness is over. They may benefit from pharmacological interventions and should see a neurologist for consultation.
An acute vestibular presentation in COVID-19 patients is “COVID-19 induced neuritis” of the vestibular nerve. These patients have sudden-onset severe vertigo, nausea, vomiting, and difficulty walking, without typical symptoms of fever or cough. These patients often need hospitalization and medical management before getting referred to vestibular rehabilitation.

Vestibular rehabilitation is effective in reducing symptoms of vertigo, visual-head motion sensitivity, and motion sickness. Exercise programs are designed to help overcome the false perception of movement due to errors in signals between the inner ear and the brain and to regain normal balance reactions. Coronavirus has challenged our lifestyles, health, and emotional well-being. Medical professionals and researchers continue to gather new information about the COVID-19 virus and how to manage post- COVID symptoms. Lingering symptoms of COVID such as dizziness, pain, and shortness of breath can continue to disrupt your life and limit you from returning to your normal activities. If you are experiencing any of these symptoms, consider a consultation at WWSPT with our Vestibular Physical Therapists.
Wendy Webb Schoenewald, PT, OCS, at
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA., 215-489-3234, wwspt@wwspt.com