Low back pain, #LBP, is one of the most common injuries people experience and get treated for in Physical Therapy. According to a study published by Georgetown University, nearly 65 million Americans report a recent episode of back pain, and some 16 million adults are limited in certain everyday activities due to chronic back pain.

The most common diagnoses of low back injuries seen in physical therapy are osteoarthritis, degenerative disc disease, strains/ sprains, disc herniations, and sciatica. These diagnoses are especially prevalent among people over the age of 40. Often, an X-ray, MRI, or CT scan is needed to confirm one of these diagnoses. However, just because one of these diagnoses is present in the lower back doesn’t mean it is the root cause of pain.
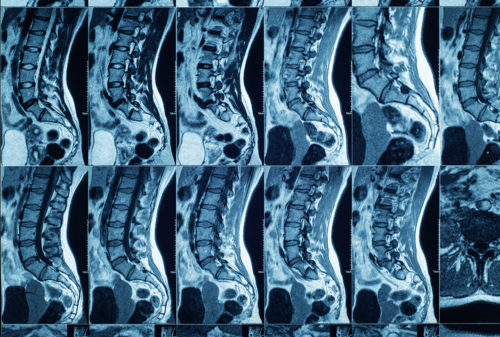
Imaging does not always correlate with symptoms. In a research study published in the American Journal of Neuroradiology, researchers took MRI images and CT scans of spines in groups of people ages 20 to 80 years old without pain. They found that about 37% of the 20-year-olds and approximately 96% of the 80-year-olds had disc degeneration. Researchers also found that among the 20-year-olds, about 30% had evidence of disc bulging or disc herniation, while 85% of the 80-year-olds had it. While the imaging revealed something abnormal about the participants’ spines, they did not report any pain.

However, some people with one or both of these diagnoses have pain. So, what is the difference if two people have the same diagnosis, but one is experiencing pain, and the other is not?
Even though two people may have the same diagnoses, their presentation is never identical; no two people have the same medical histories, comorbidities, work conditions, personal activities, and habits. As a result of these factors, different muscles are being used more often than others, which leads to asymmetries of the body. If muscles are weak or inflexible, the other muscles of the body have to compensate for those imbalances, which results in improper movement patterns and pain.
If there was no traumatic event like a car accident, odds are the structural change, like the disc bulge, was there long before the pain started. The area could have been irritated with a small movement, but it was enough to cause an exacerbation of symptoms. This is often true when someone suddenly falls or shovels for the first time in the season. The pain may dissipate when this acute irritation calms down, but the same disc bulge or degeneration remains. For some, though, the pain can become chronic and persistent.
In Alie Ward’s podcast “Ologies,” the Dolorology episode, she interviews Dr. Rachel Zoffness, a pain psychologist, about chronic pain. She discusses chronic pain as “a biopsychosocial phenomenon.” Pain is influenced by biomedical (i.e., structural changes to the body), psychology (i.e., trauma, depression, mood), and social factors (i.e., environment, accessibility), and all of these factors should be considered when treating chronic pain.
Dr. Zoffness also discusses the use of opioids for chronic pain. The opioid epidemic has become a major topic because of the many overdose deaths. While these medications can block pain messages effectively, they desensitize the brain to pain and the effects of the drug. The brain gets accustomed to the medication and then demands a higher dose to decrease pain and keep it manageable. In another scenario, the pain signals can return with a vengeance if a dose is missed.
Research shows that opioids are ineffective in long-term low back pain, but exercise and activity are effective. For those who have pain with everyday tasks, their brain is very sensitive to pain because of how long pain has been present. The brain is very good about protecting the body, so it sends “danger” messages when doing tasks like unloading the dishwasher, even though they are not dangerous. So small bouts of exercise and activity lead to desensitization of the body and reteach the brain that these tasks are normal.
Addressing the mental state is also important when dealing with long-term pain. If someone is in a bad mood or stressed out, pain can be more intense due to the brain chemicals released when he or she is not feeling good. For instance, when you’re not feeling well, your body feels so much heavier and achy. Exercise can release endorphins and dopamine to boost mood and make you feel good.

So, what exercises or movements are appropriate for back pain? Physical therapists are movement experts and will be able to evaluate and assess your pain. Many of the diagnoses listed earlier are treatable with physical therapy, but at WWSPT, we don’t just treat the diagnosis; we treat the person. We will evaluate your movement, strength, and flexibility. We will take into consideration your past medical and social history. From that information, we will develop a plan for you to become pain-free and return to your prior level of function.
Dr. Amanda Nguyen. PT. DPT,
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA.