
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, Pennsylvania
Healing, Function, Recovery, Health

Introduction
Vestibular agnosia is a rare and intriguing neurological condition that affects the brain’s ability to process vestibular information, which is critical for balance and spatial orientation. Understanding vestibular agnosia is crucial for medical professionals, researchers, and those affected despite its rarity. This blog aims to provide a detailed overview of vestibular agnosia, including its symptoms, causes, diagnosis, and treatment options.
What is Vestibular Agnosia?
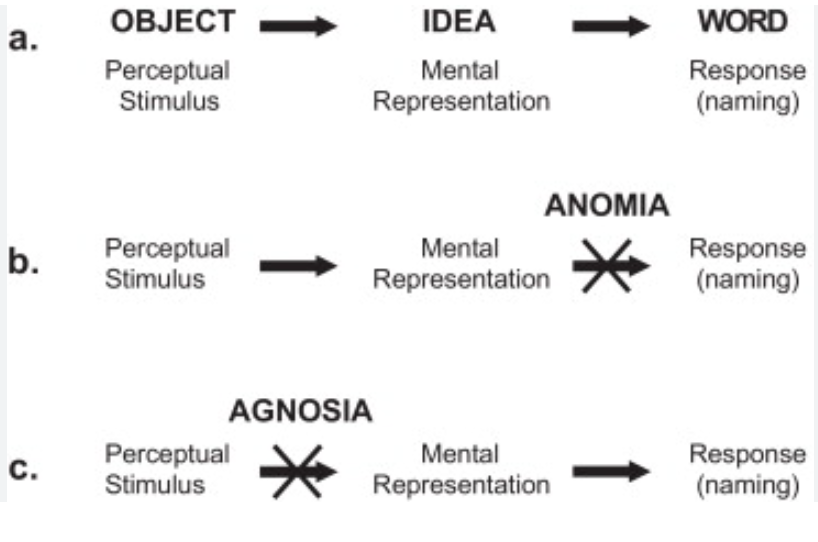
Vestibular agnosia is a neurological disorder characterized by the inability to recognize or process vestibular stimuli. The vestibular system in the inner ear plays a fundamental role in maintaining balance, spatial orientation, and coordinating movement. Individuals with vestibular agnosia have intact vestibular function but cannot consciously perceive or interpret vestibular information, leading to significant difficulties in everyday life.
Symptoms of Vestibular Agnosia
The symptoms of vestibular agnosia can vary widely but often include:
Causes and Risk Factors
The precise cause of vestibular agnosia is not fully understood. Still, it is typically associated with damage or dysfunction in the brain areas responsible for processing vestibular information, such as the parietal lobes or the temporoparietal junction. Potential causes and risk factors include:
Diagnosis
Diagnosing vestibular agnosia involves a comprehensive evaluation by a Neurologist or a Vestibular Physical Therapist specializing in vestibular disorders. The diagnostic process typically includes:

Treatment and Management
Currently, there is no cure for vestibular agnosia, but several treatment approaches can help manage the symptoms and improve quality of life:
Conclusion
Vestibular agnosia, while rare, presents significant challenges for those affected. We can enhance our understanding and management of this complex condition through continued research and advancements in diagnostic and therapeutic techniques. Healthcare professionals must remain vigilant in recognizing the signs of vestibular agnosia to provide timely and effective support for their patients.
Raising awareness and improving education about vestibular agnosia can contribute to better outcomes and quality of life for individuals living with this condition. Suppose you suspect that you or a loved one may be experiencing symptoms of vestibular agnosia. In that case, seeking professional medical advice for a comprehensive evaluation and appropriate management is essential. Contact WWSPT for additional information on Vestibular agnosia and/or to schedule an evaluation,
Wendy Webb Schoenewald, PT, OCS,
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA.
(215) 489-3234
There are four primary motor symptoms of Parkinson’s disease:
Observing two or more symptoms listed above is the main way physicians diagnose Parkinson’s. However, it is important to know that not all of these symptoms must be present for a Parkinson’s diagnosis.
Tremor tends to occur at rest and is a slow, rhythmic movement that typically starts in one hand, foot, or leg and eventually affects both sides of the body. Alternatively, some people with Parkinson’s disease will also experience an internal tremor, which is not necessarily noticeable to others. I have had patients describe this as feeling like their phone is vibrating in their pocket even though it is not there.

Rigidity refers to stiffness or tightness of the limbs or torso not associated with arthritis or orthopedic problems. Recognizing this symptom early is important to begin completing a daily stretching routine to slow the progression and maintain a more upright posture.
Bradykinesia is a very common symptom of Parkinson’s disease, which presents as an overall slowness of movement. One of the manifestations of bradykinesia is a reduced arm swing that can occur in one or both arms while walking. Other demonstrations of bradykinesia are mask-like expression of the face, difficulty buttoning a shirt or putting on a jacket, and slow, small handwriting.
Postural Instability, or difficulty balancing, is the inability to maintain a steady, upright posture or to prevent a fall, which tends to be more pronounced in the later stages of the disease. These balance problems may lead to a greater tendency to fall backward, commonly seen when attempting to stand from a chair or step backward. Postural instability may also lead to gait difficulties. Common examples are slow, small steps or a shuffling gait, also known as festination, or the very opposite, which can be seen with a tendency to propel forward with quick, short steps. Episodes of freezing are another common gait abnormality where the feet may appear stuck or glued to the floor despite attempts to take a step.
Early speech, occupational, and physical therapy interventions are key in managing this disease progression. If you or a loved one notices these symptoms or changes in movement, it is important to participate in physical therapy and a daily exercise routine to address these motor symptoms before they start affecting daily activities. Here at WWS Physical Therapy and Vestibular Rehabilitation, we have several therapists specializing (with specific training and experience) in treating those with Parkinson’s disease and other neurological disorders.
Dr. Karli Lynch, PT, DPT,
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA.,
(215) 489-3234
Young-onset Parkinson’s disease – The Letter Y in The ABCs of Parkinson’s Disease
It’s not common to see Parkinson’s disease in younger people, but for a small subset of sufferers, the disease strikes early. Young-onset Parkinson’s Disease (YOPD) occurs in people younger than 50 years of age. Most people with typical Parkinson’s disease (PD) develop symptoms at 50 years of age or older, but YOPD affects about 4% of the one million people in the U.S. with Parkinson’s disease. For example, Michael J. Fox was diagnosed with YOPD at just 29 years old.

How is young-onset Parkinson’s disease different?
Those with YOPD more frequently have a family history of Parkinson’s disease. They also tend to have longer survival. People living with young-onset Parkinson’s disease may have slower symptom progression and less frequent cognitive problems. On the other hand, they also tend to experience more side effects from medication treatments like dyskinesias (involuntary body movements) and earlier and more frequent dystonia (cramping of muscles and abnormal postures).

It is important to distinguish young-onset Parkinson’s disease from typical Parkinson’s disease because people who are affected by PD at a young age experience the disease differently. They may be busy in their career or have children to care for, often leading to less time engaging in their own care. However, for those diagnosed with young-onset PD, it is important to treat the symptoms using exercise and physical therapy as early as possible. Younger brains have a greater neuroplasticity potential, which means they have a better ability to grow and change in response to physical therapy treatment and exercise. To learn more, contact WWSPT to schedule an evaluation and/or a treatment program.
Reference:
https://www.parkinson.org/abcs-pd
https://www.parkinson.org/understanding-parkinsons/what-is-parkinsons/young-onset-parkinsons
Dr. Karli Lynch, PT, DPT,
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA.
(215) 489-3234
The Importance of Physical Therapy Screening for Risk of Falling and Benign Paroxysmal Positional Vertigo (BPPV)
Falling can happen at any age and cause a person significant injury. For someone over 65 years of age, falls are especially concerning. The World Health Organization recognizes falls as the second most common cause of unintentional death in the world (after car accident-related injuries) and states that “older people have the highest risk of death or serious injury arising from a fall, and the risk increases with age.”
Physical therapists have long worked with people to figure out what is causing falls or balance problems and how to best reduce the risk of falling and improve balance. The best way to reduce injuries related to falling is to prevent it in the first place. Increased fall prevention awareness in recent decades has led to important new legislation known as the Stopping Addiction and Falls for the Elderly Act, or SAFE Act.
The SAFE Act includes a provision that primary care providers refer their patients to physical therapy for fall prevention evaluation and services if the person has fallen in the last year. Recent economic analysis of how health care is used has shown the cost-effectiveness of physical therapists’ care for fall-related services, mainly through reduced hospital and emergency room admissions. More than saving Medicare money, this bill is about improving people’s care and helping prevent injuries and death.

Referral to Physical Therapy for fall-related services is ideal because physical therapists are uniquely qualified to evaluate and treat the most common causes of falling. Balance problems can have many contributing factors, including changes in vestibular function, vision, and cognition, decreased muscle power, reduced endurance, decreased sensation in the feet and joints, and changes in coordination. Physical therapists are trained to evaluate these areas, screen for these issues, and analyze how someone walks and moves in different situations.
A vestibular physical therapist is particularly well suited to screen for benign paroxysmal vertigo, an issue that can both cause falls and be caused by falls. BPPV is an issue where tiny calcium carbonate crystals that are meant to be in one part of the vestibular system in the inner ear come loose and go into one of the semi-circular canals, which are little tubes that sense turning head movements
_____________________________________
1 https://www.who.int/news-room/fact-sheets/detail/falls
2 https://www.apta.org/news/2024/03/12/falls-legislation-safe-act
3 https://www.valueofpt.com/
_____________________________________
When the crystals move in the canals, they stimulate the inner ear and signal to the brain that the head is turning, even though it isn’t. This typically creates a false sense of movement, usually a spinning sensation called vertigo.
It turns out that not everyone who has BPPV experiences vertigo or even a dizziness sensation. Someone with BPPV may feel more off balance with movement due to the crystals being out of place but report no dizziness. When we test them with video goggles, however, we will see the classic involuntary eye movements, called nystagmus, used to diagnose BPPV accurately. Treating their BPPV through positioning maneuvers that guide the crystals out of the canals will help their balance improve.
A new study from a specialty falls and balance clinic in Melbourne, Australia, found that 1 in 4 patients they saw for falls risk who had BPPV had no symptoms of dizziness! This is a great example of why we screen people for BPPV when there is a sudden change in balance function or a recent fall–even if they do not complain of dizziness.

Of course, if a patient feels dizzy, this dizziness can also lead to a fall. Treating someone’s dizziness, understandably, will help reduce their risk of falling. This has now been supported by large-scale research. A 2023 study published in the Journal of the American Medical Association (JAMA) found that using physical therapy decreased fall risk in patients in the US who had dizziness. The study found that 7% of adults being evaluated for dizziness had a fall resulting in a medical encounter within a year of experiencing dizziness. Receiving physical therapy within 3 months of the initial dizziness visit was associated with an 86% decrease in the odds of falling.
This underscores the value of physical therapy care—particularly by a physical therapist with training and expertise in treating dizziness—for those who have fallen or feel at risk of falling or for those who are experiencing dizziness. If your healthcare provider recommends you seek physical therapy care due to a fall, following through with the therapy is in your best interest. And if you are dizzy, you can reduce your risk of falling by receiving physical therapy. The physical therapists at WWSPT would be happy to help you reduce your risk of falling and feel more confident in your balance again.
Dr. Greg Synnestvedt, PT, DPT,
WWS Physical Therapy and Vestibular Rehabilitation
Doylestown, PA.
(215) 489-3234
_____________________________________
4 Susan Hyland, Lyndon J. Hawke & Nicholas F. Taylor (2024) Benign paroxysmal positional vertigo without dizziness is common in people presenting to falls clinics, Disability and Rehabilitation, DOI: 10.1080/09638288.2024.2320271
5 Marmor S, Karaca-Mandic P, Adams ME. Use of Physical Therapy and Subsequent Falls Among Patients With Dizziness in the US. JAMA Otolaryngol Head Neck Surg. 2023;149(12):1083–1090. doi:10.1001/jamaoto.2023.2840
We strive to provide an environment of recovery and healing for our clients, to allow them to advance their health and return to function, recreation or sports. It is our belief that Physical Therapy is the initial link in the healthcare system for Musculoskeletal and Balance related issues and we are the true experts on exercise. We look forward to a long term relationship with our patients and their families over their life span and hope to become their practitioner of choice for acute musculoskeletal issues, neuromuscular issues as well as reoccurring events limiting their Wellness. We want to be a part of our patients Healthy living and Healthy aging.