In honor of Balance Awareness Week, here are Dr. Kelsey Hanlon’s Balance ABCs:

Age: Balance does tend to worsen with age as our strength, vision, hearing, and vestibular systems weaken. Luckily, balance can be improved at any age to maximize independence and maintain function.
Blood Pressure: A drop in blood pressure immediately upon standing, also known as orthostatic hypotension, can cause lightheadedness and/or unsteadiness with quick changes in position which can lead to increased risk of falling.
Confidence: Poor balance confidence is linked to an increased risk of falling. Often people who are fearful of falling perform less movement and become deconditioned which can lead to falls when they do have to move. Conversely, overconfidence or poor insight into limitations and deficits can also increase fall risk.
Dehydration: Dehydration can cause lightheadedness or dizziness and impact balance. A typical recommendation for water intake is 8 glasses per day, but this number varies depending upon age, gender, height, activity level and environment. In general, several trips to the bathroom with light yellow to clear urine indicates adequate water intake.
Environment: There are several environmental factors that can impact balance including poor lighting, uneven surfaces, throw rugs or lifted carpet edges, pets, slippery surfaces and familiarity with an environment. It is important to scan an environment for potential risk factors, especially when it is unfamiliar. Measures must also be taken at home to maintain a safe environment and decrease risk of falling.
Falls: Falls are the most serious consequence of poor balance and are the leading cause of morbidity and mortality in older adults.
Gait: People having difficulty with balance often ambulate with a wide gait (similar to a baby learning to walk). A slow gait speed is also associated with an increased risk of falling. A physical therapist can help you improve your gait to decrease risk of falling.
Hearing: We use cues from all of our senses to understand and react to our environment. Studies have shown that poor hearing is associated with balance deficits, so it is important to have regular hearing tests and wear hearing aids as prescribed.
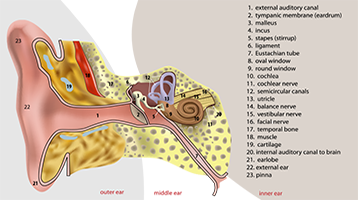
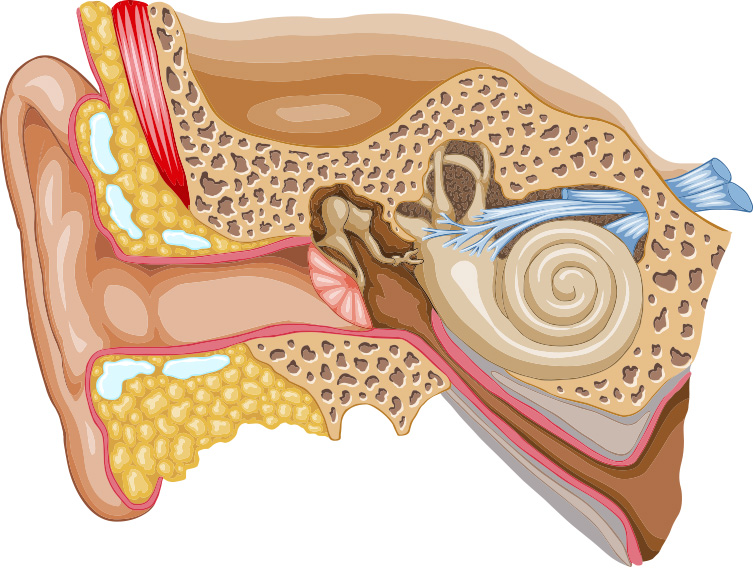
Inner ear: Your inner ear, also known as your vestibular system, is one of the 3 main systems used to maintain balance. Mechanical, structural, or neural changes to the inner ear can cause dizziness and imbalance. A physical therapist experienced in vestibular rehabilitation can help determine any deficit in your vestibular system and develop a program to improve dizziness, balance and stability.
Jumping eyes: During a vestibular or balance evaluation, your therapist will likely look closely at your eyes, sometimes using a pair of infrared goggles. We are looking for “jumping eyes” patterns, also known as nystagmus, which are involuntary eye movements created by your brain in response to feedback from your vestibular system. We rely on these eye movements to give us information about what may be happening in your inner ear, which is otherwise too small to see.
Kelsey Hanlon, PT, DPT: Kelsey, along with all of her colleagues at WWSPT, has trained specifically on treatment of balance and vestibular disorders. We are here to assist you in your dizziness and balance needs.
Lighting: Because we rely heavily on our vision to maintain balance, low light situations are more likely to cause imbalance. It is important to make sure that bedrooms, bathrooms and hallways are lit at night as well as any outdoor areas that are frequently traversed in order to decrease fall risk.
Medications: Some medications, including antiparkinsonism drugs, nitrates, antidepressants and antipsychotics can cause orthostatic hypotension as a side effect. It is important to know and understand your medications and how they may impact your balance.
No back shoes: Wearing clogs, flip flops, sandals or other shoes without a strap around the heel can lead to increased risk of falling due to slipping and/or shuffling while using this type of footwear.
Orthopedic Issues: Pain or deformity in any of the joints or muscles of your legs and trunk can disrupt your gait and balance. It is important to get these issues resolved quickly and maintain gait pattern as close to normal as possible to decrease fall risk.
Posture: Postural changes such as a forward or lateral lean in standing and walking can change center of mass and result in imbalance. A physical therapist can help guide you in appropriate exercises to maintain or improve posture.
Quick turns: Turning or moving too quickly, especially when combined with a vestibular deficit, can result in imbalance. Practicing turning and fine tuning vestibular function under the care of a physical therapist can improve balance in these situations.
Recent falls: Research has shown that there is a 50-60% increase in the risk of falling within 6 months of a previous fall, so be sure to see a physical therapist if you do fall to have a thorough evaluation.
Somatosensory system: One of the 3 main systems that your body uses for balance, this system includes sensory information from your feet as well as information from your muscles, tendons and joints to supply your brain with feedback to help you maintain balance. This system can be impacted with lower extremity injury, or sensation issues such as diabetic neuropathy.
Throw rugs: A big “no-no” in the vestibular community, these rugs tend to flip up or slide which can increase risk of falling. Remove them from your home, especially if you are elderly, to decrease risk of losing your balance.
Uneven Ground: These surfaces tend to challenge your somatosensory system and therefore make balancing more challenging. If you are unsure of yourself, uneven surfaces such as grass, rocks and hills can pose a threat to your balance, and you may want to use an assistive device such as a cane, especially if you are unfamiliar with the environment.
Vision: One of 3 of the body’s main balance systems, most people rely on their vision primarily for balance. This becomes an issue as vision decreases with age, or in low light situations. Physical therapists will have you practice balancing with your eyes closed to decrease reliance on the visual system and strengthen your other balance systems.
Wide base of support: If you know that you are in a position where your balance may be challenged, opening your feet wider will give you an advantage and make it easier to maintain balance. This is a useful tool when ambulating on particularly challenging surfaces, but if you feel yourself doing this on flat and typical surfaces you should be evaluated for your balance.
eXercise: Regular exercise will keep your musculoskeletal, circulatory and respiratory systems in top shape which helps you maintain balance. There are also specific vestibular and balance exercises that you can do to decrease risk of falling. A physical therapist will evaluate you and assign exercises to appropriately challenge you.
Yoga: Many yoga poses are designed to challenge balance. They range from beginner poses to more challenging poses and can be adapted to meet any skill level.
Zzzzz: Sleep is essential for restoring our skeletal, nervous, and muscular systems. People who do not get a good quality sleep, especially chronically, often exhibit balance deficits.