Do you have symptoms like dizziness, lightheadedness, nausea, or a feeling of being off-balance? These are all symptoms of a very common form of an inner ear disorder called Benign Paroxysmal Positional Vertigo, BPPV. It is the most common disorder of the inner ear affecting about 9% of the population over 60 years old. It is the most common diagnosis treated in my clinic, representing 30 to 40% of the dizzy patients we evaluate. Since it is associated with increased fall risk in adults, it is important to treat them promptly.
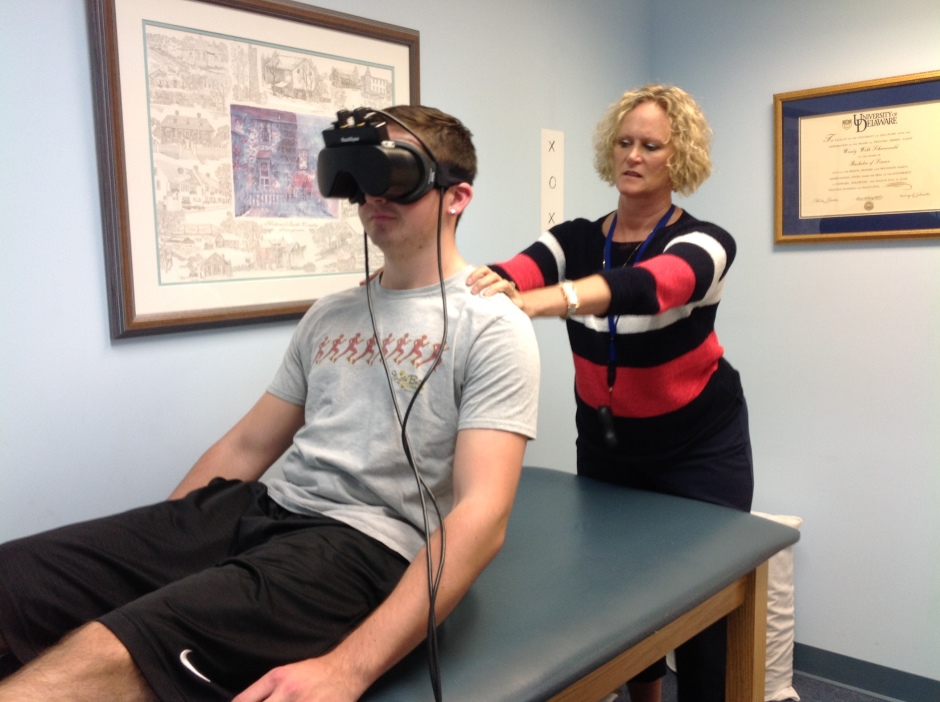
BPPV is a mechanical disorder of the inner ear that occurs when calcium carbonate crystals, called otoconia, which are normally embedded in the utricle of the inner ear, become dislodged. They migrate into one or more of the three semicircular canals, where they are not supposed to be. When this happens, the otoconia shift and create an abnormal movement of fluid in the canal, causing a false sense of rotational motion. Once the otoconia are loose, if we move our head or body, the fluid moves more quickly because of the weight of the otoconia. This causes the inner ear to send false signals to the brain that the room is spinning. This creates the illusion of motion the patient perceives as vertigo, though physiologically it causes abnormal eye movement called nystagmus, which therapists can observe to diagnose BPPV. How is it treated? Since #BPPV is a mechanical disorder of the inner ear, it can be treated quickly without medicine. A specially trained vestibular physical therapist can resolve vertigo by performing an #Epley maneuver, also called a canalith repositioning maneuver. The therapist uses a very specific series of head and body movements to guide the otoconia back to the utricle where they belong. Sometimes, the otoconia are found to be in a different canal or are adhered to the cupula. This will then require the use of a different maneuver for treatment, but your therapist will be able to determine this through observations during the exam.

Though patients can commonly be treated effectively with the Epley maneuver, the recurrence rate for BPPV is high. Since its symptoms are not very pleasant, patients who suffer from vertigo do not like to hear that there is a 10 to 18% chance of another attack within the next year. The recurrence can vary greatly; patients might have another attack within 6 months or 6 years.
How can I prevent recurrent attacks?
The etiology of BPPV is unclear, but a recent systematic review of research articles from 14 countries looks at risk factors affecting the recurrence of BPPV. The risk factors identified may help us identify fall risk patients and help clinicians educate patients about the importance of follow-up after BPPV diagnosis.
Women are more likely to relapse than men, which may be related to menopause causing changes in hormone levels. Patients older than 65 years are more likely than their younger peers to suffer from BPPV. Osteoporosis has been found to be common in patients with BPPV. Age-related decline in calcium metabolism may also affect the otoconia, weakening their structure, which causes them to break off and allows them to float freely. Treatment of osteoporosis may have a protective effect against BPPV. This study also suggests that systemic diseases, including hypertension, hyperlipidemia, and diabetes mellitus, could increase the incidence of relapse attacks. This may be related to the known effect of vascular disease on the inner ear. These diseases can affect microcirculation, causing ischemia or reduced blood flow to the inner ear. It is important to monitor your glucose, A1C readings, and blood pressure and follow your doctor’s recommendations for the management of these disorders.
History of migraines is a strong risk factor for relapse of BPPV which can have a vascular factor that can damage the inner ear making recurrent BPPV more prevalent. Common inner ear disorders, such as otitis media and Meniere’s disease, increase the incidence of BPPV by disrupting the normal function of the semicircular canals.
In head trauma, 13% of patients report positional vertigo and have bilateral disease at a higher rate than idiopathic attacks of BPPV. Another risk factor that is a common problem with aging adults is cervical spondylosis and limited mobility of the spine, which makes BPPV treatment maneuvers more difficult to perform.
These risk factors for the recurrence of BPPV help us measure fall risk in patients and help clinicians educate patients about the importance of follow-up after BPPV diagnosis. Regular aerobic exercise can be helpful in managing all these disorders and in keeping the vestibular system healthy. Medical management from your primary physician is important in managing the systemic conditions. A thorough discussion about your medical history with our clinicians helps us customize a treatment and education program specific to you. Although we love what we do in fixing dizzy patients, we want to teach our patients to have confidence in managing and preventing their own symptoms.
Wendy Webb Schoenewald, PT, OCS
WWS Physical Therapy & Vestibular Rehabilitation
Doylestown, PA
215-489-3234

I recently had an episode of this. I googled it and was pretty sure it was BPPV. I don’t believe there’s any possibility of seeing my primary care doctor the same day. I called an urgent care place and was advised to go to the ER, where I had two brain CTs with contrast, spent the night in an ER room, had an MRI in the morning, then got into a room. A PT came by and I was so relieved to see her. I wish I had seen the PT first but I understand why the ER doctor took the precautions he did. I got moved around by two PTs on a table and I’m back home and much better. I could try the maneuvers myself but I’m afraid of making it worse. I have an appt with PT next week. In the meantime I’m practicing some one legged postures like tree pose and it’s getting better. It’s kind of weird and wonderful how this happens and how it’s treated. I’d never heard of it before I got it. Would like to hear more relapse prevention info