Physical Therapy for Vestibular Disorders & Rehabilitation
Vestibular Rehabilitation:
Adult Vestibular Disorders are typically underdiagnosed and undertreated. An estimated 35.4% of US adults age 40 years and older (109 million Americans) experience Vestibular Dysfunction at some point in their lives; a percentage of this group goes on to develop a chronic Vestibular Disorder. In the US, medical care for patients with chronic balance, disorders exceeds $1 billion per year. The word “Vestibular” refers to the inner ear balance system and to achieve good balance we rely on this system to coordinate our brain, eyes, inner ear, and musculoskeletal system to work together.
What are the typical symptoms and signs of a vestibular disorder?
The primary symptoms of a Vestibular Disorder include dizziness, vertigo, and disequilibrium. Dizziness is a sensation of lightheadedness or unsteadiness. Vertigo is a perception of the movement of the self or surrounding objects that most people describe as spinning and can be quite disabling. Dizziness and Vertigo can be a symptom of many Vestibular Diseases and Disorders; The WWSPT experts will evaluate the type of dizziness to help find what type of vestibular dysfunction you are having.
Disequilibrium means unsteadiness and balance that can be accompanied by spatial disorientation. And this may present itself as stumbling or difficulty walking a straight line will or turning. Other signs and symptoms include visual-spatial problems, hearing loss, frequent falls, difficulty moving in the dark, difficulty reading, difficulty concentrating, and increased anxiety.
How do vestibular disorders impact quality of life?
An estimated 33% of all adults with chronic balance problems experience difficulty performing basic activities of daily living such as bathing, dressing, eating, and walking safely without falls. We don’t notice what the vestibular system does for us until it is not working correctly. It can be very disabling for many people, though we can manage your symptoms and often cure them with the proper treatment and diagnosis.
The staff members at WWSPT are the region’s experts on Vestibular Dysfunction care. No matter the diagnosis they provide the newest evidence-based medical care for our patients. We are involved with leading research in the treatment of some of the most common forms of Vertigo and teach other physical therapists how to appropriately treat Vestibular patients.
Common vestibular disorders include:
- Benign Paroxysmal Positional Vertigo
- Labyrinthitis Neuronitis
- Ménière’s Disease
- Acoustic Neuroma Tumors
- Vestibular Migraine
- Cervical Vertigo
- Peripheral Neuropathy
- Disequilibrium of Aging
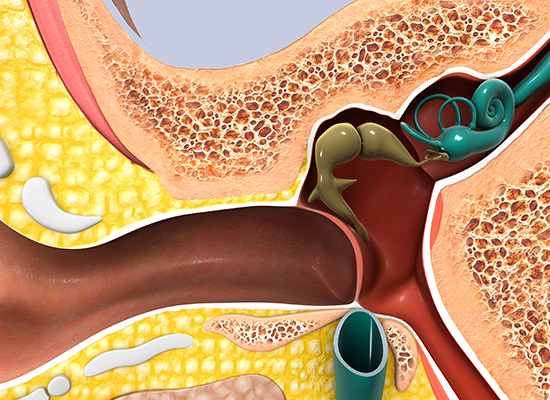
BPPV is the most common disorder of the inner ear, which is a vital part of maintaining balance. BPPV produces a sensation of spinning called vertigo that is triggered by positional changes or sudden movements and changes in head position.  BPPV fee is benign and not life-threatening or progressive, but can be quite disabling. BPPV occurs when otoconia, tiny crystals of calcium carbonate that are a normal part of the inner ear’s anatomy, detach from the utricle and usually collecting in the posterior semicircular canal due to gravity. When the head moves the otoconia shift stimulating a sensor to send false signals to the brain producing Vertigo and a jerking movement of the eyes called Nystagmus.
BPPV fee is benign and not life-threatening or progressive, but can be quite disabling. BPPV occurs when otoconia, tiny crystals of calcium carbonate that are a normal part of the inner ear’s anatomy, detach from the utricle and usually collecting in the posterior semicircular canal due to gravity. When the head moves the otoconia shift stimulating a sensor to send false signals to the brain producing Vertigo and a jerking movement of the eyes called Nystagmus.
In Classic BPPV head movements, such as looking up or down or rolling over and getting out of bed can trigger Vertigo attacks that lasts seconds to minutes. Symptoms can also include dizziness lightheadedness, nausea and balance as well as difficulty concentrating. Episodes may be experienced for short duration but can frequently occur almost daily until properly treated.
The most common cause of BPPV is head injury and may be the result of a concussive force that displaces the otoconia. In people over age 50, it commonly occurs for no specific reason but is thought to be associated with the natural aging process of the otolithic membrane. B PPV has been associated with migraine and ototoxicity as well as viruses that can affect the ear. it occasionally follows surgery and a prolonged period of bed rest.
BPPV is diagnosed based on medical history, physical exam and Dix halpike manuever which allows a physical therapist to elicit nystagmus in response to change in head position the problematic semicircular canal can be identified based on the observed nystagmus. This test is performed with video goggles, and called FRENZEL lenses, will that magnify the eyes and illuminate the nystagmus for more accurately diagnosis.


Treatment of Vertigo employs Canalith Repositioning Maneuvers that move the displaced otoconia out of the affected semicircular canal back to their original site . This is called an Epley maneuver, which involves a specific series of pattern head and trunk movements that can be performed in approximately 15 minutes to resolve the vertigo on the initial evaluation visit. The Epley maneuver is more effective than medication and can often successfully be completed in one visit 90% of the time. There are three canals on each ear where the otoconia can be displaced and there are different maneuvers for each canal. Treatment by our Vestibular Physical Therapists, who have special training in diagnosing and in performing all of these maneuvers is essential to achieve resolution of Vertigo, dizziness and balance symptoms in as few visits as possible. However even with successful treatment, B PPV can reoccurs in one third of the patient’s after one year and 50% of the patient’s after five years.
For Self-Treatment of BPPV – Right DOWNLOAD WWSPT’s BPPV Canalith Repositioning Maneuvers – Right below:
For Self-Treatment of BPPV – Left DOWNLOAD WWSPT’s BPPV Canalith Repositioning Maneuvers – Left below:
Vestibular Migraine:
Migraine is one of the most debilitating chronic disorders in the US is more common than Asthma and Diabetes more importantly Migraine strikes people during their most productive years between ages of 20 to 40, and affects more women than men. Despite better diagnostic capabilities and efforts to improve public awareness it is estimated that 50% of migraineurs go undiagnosed. Migraine is typically characterized by unilateral onset of head pain, severe intensity of pain, throbbing or pounding and interference with the person’s routine activities. Symptoms can include photophobia, which is a sensitivity to light, or photosensitivity, intolerance to noise, and nausea and vomiting. Approximately 40% of migraine patients have vestibular symptoms associated causing loss of balance or dizziness. B PPV can also be triggered by Migraine, this is thought to be caused by a combination of vascular events along with alteration in neural activity associated with the migraine event. Persons with Vestibular migraine often do not have the true headache symptoms but more of the vestibular symptoms and this makes diagnostic evaluation difficult because physicians often expect the classic migraine symptoms.
These patients can be effectively treated by Vestibular Physical therapist after thorough evaluation and treatment along with medical management by a physician to find the right combination of medication that can control the Migraine attacks. Our specialists will develop exercises to gradually increase the patient’s abilities the program and has to be carefully administered with exercises that her properly dosed so as not to trigger another migraine event. Treatment often includes education about diet and lifestyle modifications.
Cervical Vertigo:
When patients have cervical pain they often do not move their head and neck as much, this can lead to vestibular dysfunction or sensitivity to movement causing episodes of dizziness and lightheadedness. Concussion Injuries can also involve Cervical injuries. Physical therapists are trained to evaluate the musculoskeletal system and further evaluate cervical movements that can be triggering dizziness as well as pain. Often manual therapy treatments and vestibular exercises can help resolve cervical vertigo.
Ménière’s Disease:
Meniere’s Disease is another common vestibular dysfunction that is thought to be caused by a plumbing problem in the inner ear. When too much fluid builds up there can be a traumatic release of this fluid causing a Vertigo attack that can last between 4 to 12 hours. He these patients can also often have sensitivity to movement and balance and dizziness that a Vestibular Physical Therapists can evaluate and provide specific treatment to resolve the symptoms.
Acoustic neuromas also known as vestibular Schwan no months , our nonmalignant tumors of the eighth cranial nerve commonly causing hearing loss and gradual decline in balance. Because these tumors are very rare and slow growing they are usually found on MRI imaging. Physical therapy and vestibular rehabilitation are needed postoperatively to regain adaptation of the vestibular system.
Dizziness and Balance; ACOUSTIC NEUROMA
Vestibular Neuritis and Labyrinthitis:
In vestibular neuritis, dizziness is attributed to a viral infection of the vestibular nerve (see figure 1). The vestibular nerve carries information from the inner ear about head movement. When one of the two vestibular nerves is infected, there is an imbalance between the two sides, and vertigo appears. Labyrinthitis, is defined as the combination of the symptoms of vestibular neuritis, with the addition of hearing symptoms. It may be due to a process that affects the inner ear as a whole, or due to a process that affects the 8th nerve as a whole. Labyrinthitis is also always attributed to an infection. The symptoms of both vestibular neuritis and labyrinthitis typically include dizziness or vertigo, disequilibrium or imbalance, and nausea. Acutely, the dizziness is constant. After a few days, symptoms are often only precipitated by sudden movements. A sudden turn of the head is the most common “problem” motion. While patients with these disorders can be sensitive to head position, it is generally not related to the side of the head which is down (as in BPPV), but rather just whether the patient is lying down or sitting up.
It usually takes 3 weeks to recover from vestibular neuritis or labyrinthitis. Recovery happens due to a combination of the body fighting off the infection, and the brain getting used to the vestibular imbalance (compensation). Some persons experience persistent vertigo or discomfort on head motion even after 3 weeks have gone by. After two to three weeks a referral to a vestibular rehabilitation program, may help speed full recovery via compensation. You can DOWNLOAD the PDF guides below to learn more about Vestibular Neuritis and Labyrinthitis:
Computerized Balance testing with Neurocom Balance Master
Falls are common in those with vestibular dysfunction and can have serious consequences when they result in injury, therefore it is important to prevent them as much as possible .To thoroughly assess balance deficits we use a computerized assessment with a balance master to provide objective data regarding sensory input and postural control. This enables our therapists to develop a more effective program to prevent falls or improve your balance. The assessment data is maintained in our system and compared to age normal’s therefore giving you a measure of your abilities compared to your peers. It can also be compared internally on future visits to demonstrate improvement or on yearly evaluations to prevent decline in balance ability. The test is similar to a Wii game except the data is collected and can be compared during each session. This can help us evaluate your fall risk and help us develop a fall prevention program tailored specifically to you.

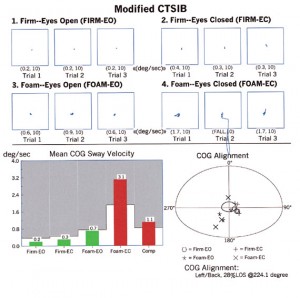
Balance Master Tests Include:
Sensory integration testing evaluate your sensory systems, specifically how your vestibular, vision and proprioceptive systems affects on your ability to maintain balance.
Limits of Stability:
Evaluates motor control and accuracy of movement with speed and displacement of the body at a target this is a measure of neurological systems ability to coordinate together properly.
Rhythmical Weight Shift:
Evaluates one’s ability to dynamically control weight shift anterior and posterior as well as medial-lateral at varying speeds with specific patterns. This is also a measure of neuromuscular coordination
Are you at risk for a fall? Does “dizzy” mean “off-balance” to you? – Take our Self Test