Physical Therapy for Vestibular Migraines
A migraine is a neurologic event that results in symptoms such as headache, dizziness, nausea, and increased sensory sensitivity. Migraines wreak havoc on the sensory systems, causing sensitivity to light, smells, sound, and motion. These symptoms are typically severe enough to interfere with daily function and cause a person to lie down. While an episode can last anywhere from a few minutes to 72 hours, there can be lingering symptoms or symptoms between episodes that can last weeks to months.
Migraines impact specific brain areas, accounting for various vestibular symptoms. While some types of migraines involve a headache, it is important to note that a vestibular migraine may or may not involve any headache. A vestibular migraine episode typically includes dizziness, trouble walking or standing, a spinning sensation, motion sensitivity (like car sickness), lightheadedness, or imbalance. The episodes can also cause nausea and vomiting. Vestibular migraine can be challenging to diagnose. Often, doctors order various tests, all of which return with expected results.

According to the Vestibular Disorders Association (VeDA), vestibular migraine is estimated to impact 1-3% of the population, and 40% of all migraineurs have some accompanying vestibular symptoms. Fifty percent of people with migraines go undiagnosed or are mismanaged. Those who suffer from vestibular migraines most often have a history of “typical” migraines earlier in life. However, the onset of vestibular migraine tends to be later in life compared to traditional migraines. There is evidence to suggest there is a genetic predisposition to having a “migrainous brain,” so often, there is an identifiable family history of some form of migraines in those who experience migraines.
Role of Vestibular Rehabilitation Therapy
Vestibular rehabilitation can play an essential role in the differential diagnosis of vestibular migraine, which is commonly misdiagnosed as other vestibular issues. We provide education in migraine management and resources to better understand the diagnosis. Education about lifestyle management can help prevent episodes and lower the threshold to trigger a migraine (making the brain less vulnerable to an attack). Improving awareness of staying hydrated, maintaining regular sleep patterns, and eating small meals throughout the day can be very helpful in maintaining homeostasis in the body and avoiding episodes. Vestibular rehabilitation focuses on managing motion or visual motion intolerance through desensitization of triggering stimuli to improve sensory processing and promote balance retraining. Aerobic exercise also has evidence to be beneficial in preventing vestibular migraines and associated symptoms. The most effective treatment of chronic migraine is often a combination of medication, vestibular therapy, and lifestyle modification.
Typical Migraine Course
Migraine can include 4 phases (not every individual experiences every phase):
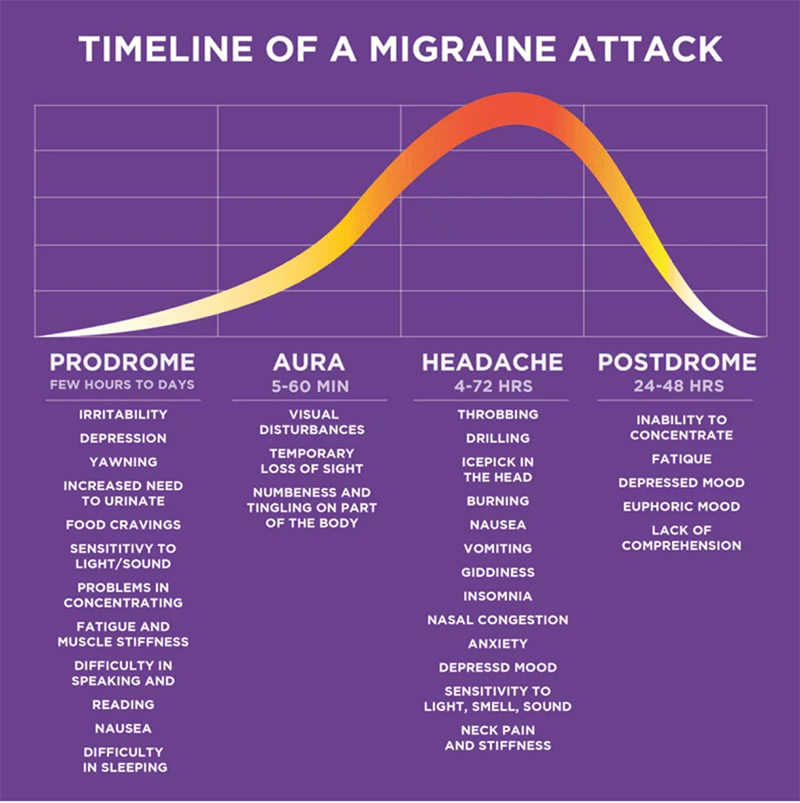
1) Prodrome—This can last a few hours to days before the headache and can include increased neck pain, yawning, increased urination, increased sensitivity to light, scents, and sound, depression, irritability or mood change, nausea, difficulty with speech and reading, and reduced concentration.
2) Aura – can last anywhere from 5-60 minutes and often precedes the migraine. There is a misconception that if you don’t experience aura, you don’t have migraines, but this is untrue. The most common type is a visual aura, which involves seeing a flashing lightning bolt, zig zag, sparkles, or a blind spot in your visual field. Other individuals experience a sensory aura, which can include transient numbness or tingling in the face or upper extremity, and motor auras, which include temporary changes in speech. In rare cases, temporary weakness on one side of the body is also possible.
3) Headache—This is not always present in vestibular migraine, but if it is, it is usually on one side of the head or face. It may be experienced as acute dizziness or imbalance, typically lasting 30 minutes to -72 hours.
4) Postdrome – consists of residual discomfort and “washed out” feeling, dizziness, neck stiffness, body aches, difficulty concentrating, continued hypersensitivity, and fatigue which lasts about 24 hours. This is also called the interictal stage, referring to the period between migraine attacks when a person is not experiencing an acute migraine episode but may experience these other lingering symptoms.
Tips to Conservatively Manage Migraine
Conservative management of migraine refers to reducing episodes without the use of prescribed medications. By making some behavioral and lifestyle changes through regular sleep and meal patterns, dietary changes, reducing stress with relaxation or breathing techniques, regular exercise, motion exposure, and balance training, you can lower the threshold for triggering a migraine. Migraine triggers differ for everyone, but being aware of your sensitivities can help you recognize patterns and reduce symptoms. Being aware of the first two phases can prevent the migraine from worsening. By identifying your risk factors or triggers, you can monitor and make appropriate changes to help reduce the frequency or severity of migraine events. In some cases, when migraine frequency interferes with your daily life, you may need to discuss medication options with your doctor while also considering these behavioral changes discussed below.
Stress Management
Stress is a common trigger for migraines, so it is essential to recognize stressors in your life and develop effective coping mechanisms. Relaxation programs, deep breathing, and yoga can be learned to help reduce stress. Meditation apps are a great resource, and many are available free on your phone. During a busy day, remember to take breaks to catch your breath, hydrate, and calm your mind.
It is unrealistic to expect to live a stress-free life, which makes finding effective stress management strategies an essential component of migraine management. If you are unable to cope with your stress effectively, it may be beneficial to consult a mental health professional who can help you strategize ways to reduce anxiety.

Regular exercise can help to manage stress and anxiety and reduce migraine frequency and symptom severity. In some cases, exercise is just as effective in migraine management as medication. Low-level Aerobic exercise, or exercise that makes you a little tired and sweaty is most beneficial. This could include walking, swimming, running, bicycling, rowing, yoga, exercise classes, or any other exercise where you experience an elevated heart rate. Often, migraineurs need to build up aerobic tolerance more gradually than others and your therapist can guide you as you progress through a new exercise program. Choosing an activity that you enjoy will make it more likely that you stick with the program. Studies have shown that 40 minutes of aerobic exercise 3x per week can help reduce the need for medication to manage migraines. This can be an excellent activity goal for those with migraines.
Weather changes
Some individuals notice their episodes occur in conjunction with changes in barometric pressure. Although we have no control over this, if you see a change in the weather and begin to feel symptoms, you can prophylactically manage those symptoms.
Reduction of Visual Stimuli
For some people, migraines are triggered by eye strain from exposure to bright lights or contrasting lighting, such as a glowing screen in a dark room. Photophobia is an increased sensitivity to light that is experienced by many migraine sufferers both before and during migraine episodes. Wearing sunglasses and/or a hat can be very helpful in preventing migraine or reducing the severity of symptoms during an event. Fluorescent lighting in offices and stores can be irritating, and for some, an easy solution is magnetic fluorescent light covers to reduce glare from these lights. Spending excessive time in front of a screen (such as a computer, phone, or iPad) can cause eye strain and trigger migraines. There are several options for decreasing screen brightness and/or wearing filtering or blue light glasses to reduce eye strain from screens. Use of the 20/20/20 rule can also benefit those who are triggered by screen time. This rule recommends that for every 20 minutes spent on the computer, you should look at something 20 feet away for 20 seconds.
Many people with migraines can also be triggered by busy visual stimuli such as “busy” backgrounds or fast-moving objects in a visual field (such as Imax theaters or large TVs viewed too closely), walking through crowds or a grocery store or windshield wipers when it is raining. It is essential to recognize these situations as potential triggers. A physical therapist can help assist you in slow exposure to these types of visual environments to improve your tolerance.
Addressing Motion Sensitivity
Vertiginous symptoms during and after movement are the second most common type of aura associated with migraine. Migraine sufferers often have a highly sensitized nervous system that does not tolerate quick head and/or body movements or mismatches between visual and physiologic movement. This makes them more prone to car sickness and less likely to tolerate spinning motions. Exposure to these types of activities can result in dizziness and nausea and even trigger a migraine. However, if fear and anxiety over triggering symptoms cause a person to avoid these types of movements altogether, the individual becomes more sensitive, even to everyday head movements. This can cause even small motions of the head, such as turning your head to talk to someone while walking, to result in dizziness and imbalance. It may also cause symptoms when getting in or out of bed and/or rolling over.
A vestibular physical therapist can help desensitize your body and improve motion tolerance through slow exposure exercises specific to your triggers. Some individuals experience increased motion sensitivity following a migraine event and will also benefit from systematic desensitization exercises to return to baseline.
Sleep Hygiene
Getting a proper night’s sleep is an essential practice for healthy living. Good sleep can potentially prevent chronic conditions by supporting the immune system, reducing pain perception, and improving overall quality of life. Poor sleep habits and quality have been shown to trigger migraines.
It is important to establish regular sleep hours by waking up and going to bed at about the same time every day and consistently getting 7-8 hours each night. To promote better sleep, try listening to soothing music or taking a warm bath at the end of the day to help you relax. Watch what you eat and drink before bedtime since caffeine, nicotine, and alcohol can interfere with sleep. Please refer to our “Tips for Good Sleep Hygiene” handout for more information.
Over-the-Counter Medications and Supplements
How often do you reach into the medicine cabinet each week for over-the-counter medication management for migraines? Most migraine sufferers do this more than they realize. The underlying headache or migraine must be managed to manage the dizziness, which could require medication management. Speaking with your doctor can help determine if a daily preventative medication or an as-needed abortive medication when you feel a migraine coming is proper for you. If you are hesitant to jump into medication management, exercise has been proven in many studies to be as effective in the management of migraine as medication.
Note: Always discuss any new medications or supplements with your doctor and/or pharmacist before taking them.
